About TScan
History of TCR Therapy
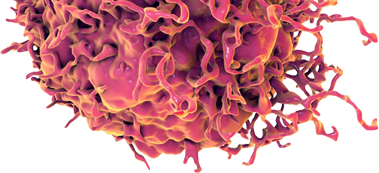
TCR T-cell therapy is one of the most promising approaches to cancer therapy, but has seen limited use due to the lack of identified targets and the lack of safe and effective TCRs. TScan seeks to build on landmark discoveries in cancer immunology by expanding the sphere of known targets and extending TCR T-cell therapy to broader populations of eligible patients.
1988
First use of T cells for cancer therapy
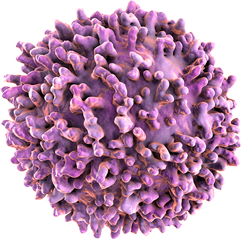
Steven Rosenberg extracts tumor-infiltrating lymphocytes (T cells) from the tumors of patients with metastatic melanoma, expands these T cells in vitro, and infuses them back into the patients. Tumor regressions are observed in over 50% of patients, demonstrating for the first time that T cells in patient tumors have the potential to fight the patient’s cancer if the T cells can be reinvigorated and amplified appropriately.
(N Engl J Med 1988, 319, 1676)
1991
First shared antigen target identified
Boon and coworkers identify the melanoma antigen gene MAGEA1, which encodes an antigen recognized by T cells, from the blood of a patient with melanoma.1 Three years later, Kawakami et al. show that TILs isolated from melanoma patients recognize the melanocyte differentiation proteins MART-1 and gp100.2 Collectively, these discoveries demonstrate the existence of productive, anti-cancer T cells that recognize non-mutated shared antigens.
1 (Science 1991, 254, 1643)
2 (Proc Natl Acad Sci USA 1994, 91, 3515; Proc Natl Acad Sci USA 1994, 91, 6458)
2006
First tumor regression using autologous T cells transduced with a TCR
Tumor regressions are observed in melanoma patients after transducing autologous T cells with a TCR recognizing the melanocyte differentiation antigen MART-1.3 More robust responses are later observed in clinical trials of an affinity-enhanced TCR targeting the cancer/testis antigen NY-ESO-1.4 Together, these trials demonstrate that robust responses in solid tumors can be achieved by introducing defined TCRs with specificity for shared antigens into a patient’s autologous T cells.
3 (Science 2006, 314, 126)
4 (Clin Cancer Res 2015, 21, 1019; J Clin Oncol 2011, 29, 917; Nat Med 2015, 21, 914)
2011
First approval of an immune checkpoint inhibitor
US FDA approves the anti-CTLA-4 antibody ipilimumab (Yervoy®) as a treatment for unresectable or metastatic melanoma. Approvals of the anti-PD-1 antibodies nivolumab (Opdivo®) and pembrolizumab (Keytruda®) follow. Immune checkpoint inhibitors function by inhibiting the immunosuppressive environment of the tumor, enabling the patient’s own T cells to mount an anti-tumor response. Collectively, this class of therapeutic agents shows that, for patients that have T cells with the appropriate anti-tumor recognition properties, dramatic and durable responses can be achieved.
2017
First approvals of genetically engineered T cell therapies
US FDA approves the CAR T-cell therapies tisagenlecleucel (KymriahTM) and axicabtagene ciloleucel (YescartaTM) for the treatment of patients with B-cell acute lymphoblastic leukemia and large B-cell lymphoma, respectively. These cell therapies work by genetically engineering a patient’s own T cells to produce a chimeric antigen receptor (CAR) that acts as an artificial T cell receptor, redirecting the patient’s T cells to recognize and eliminate their cancer cells. These approvals pave the way for future T cell therapies, including TCR T cell therapies.
2019 and beyond
Expansion and wide-spread adoption of TCR T-cell therapy
Expanding TCR T-cell therapy to a wide range of cancer indications and HLA types requires the discovery of new shared targets and safe and effective TCRs. At TScan, we are addressing this unmet need using our proprietary genome-wide, high-throughput target ID platform. Building on these landmark discoveries, we aspire to transform cancer care by making TCR T-cell therapy broadly available.